Continuing our series on the impact of machine learning and artificial intelligence on the healthcare sector from this post, we will present the state of automated diagnosis models and the relatively low market impact of AI-powered solutions so far. The critical nature of healthcare services, and associated regulation, both procedural and regarding data privacy, forces a slow pace in the implementation of marketable products powered by artificial intelligence, more so if these products and models attempt to substitute critical processes currently performed by humans.
A very useful publication to start understanding the landscape of AI applications into healthcare is this article:
As indicated in the article, advanced diagnosis, as advanced decision-making tools, offers an excellent opportunity to implement AI-powered products. In addition, care pathways modeling and logistic management of hospital environments are also considered high potential areas for implementing intelligent systems. Specifically, two topics are of interest: automatic arrhythmia analysis and fetal state assessment during labor.
Then, where are the models? Where are the products? If you had to visit a hospital lately for the medical care you have, probably and depending on location, have not experienced any advanced or automated AI process. Sadly, we had to, and even the scheduling of doctor visits was manually performed and prone to error, receiving on one occasion an appointment for a day in the past. And this is happening in a country with a well-funded, functional public healthcare sector supported by equally functional private healthcare institutions. The situation for implementing AI-powered products and procedures, unless at the very top global leaders, is lacking. Is there a lack of models? No, they are even public domain.
Healthcare institutions have partnered with machine learning and artificial intelligence sites to produce open-sourced, for-prize developed models. Recently these two: the SIIM-ISIC Melanoma Classification and RSNA-MICCAI Brain Tumor Radiogenomic Classification. Although far from perfect, the results are publicly available and can form the kernel of a medical product. The gap here is no more related to the high technology challenge; it is now a problem of implementation into the current low technology system.
As examples of the images the SIIM-ISIC project was working with, we have these skin lesion images where the machine model is capable of classifying the condition into melanoma or nevus:
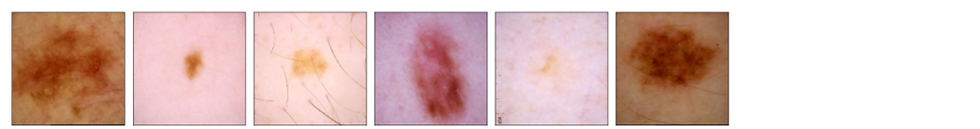
The results for the melanoma project are in this article. The out-of-sample accuracy was 95% as ROC AUC. The basic technology is here; the product and implementation are further away.
The brain tumor radiogenomic classification was even more involved, requiring the detection of genomic markers in MRI scans of 4 procedures. This data is 5-dimensional, impossible for a human to interpret:
This genomic diagnosis problem is highly complex, and the results from the competition reflected that difficulty; in any case, there is basic research done and available and not implemented.
Creating the models is difficult; this difficulty pales in comparison with these other related problems:
- Obtaining the correct, relevant data fulfilling all privacy requirements.
- Cleaning/Engineering the data.
- Validating the models. Becomes critical for diagnosis and treatment.
- Ensuring correct behavior over the complete life-cycle of the product.
- Solving ethical/social issues adjacent to AI.
There is an organizational impossibility for the healthcare sector to implement AI-powered products efficiently. No single actor in the industry has access to all the information and technology required to develop these systems in a fully compliant and safe manner. Health device companies usually lack clinical patient information while they possess device and sensor reading knowledge and deep handling expertise; hospitals have, and cannot share, clinical data linked to those sensor readings that generally are out of technical reach for medical personnel. No single actor will ever complete the engineering and regulatory trials required to get medical device level approvals.
There are thus two main gaps slowing down AI for healthcare: information accessibility and expertise fracture. Data federations are being proposed to solve the first problem, as an example this NVIDIA and King´s College proposal here:
The second problem requires better integration between manufacturers and developers with clinical organizations. Once these issues are solved, clinical validation issues and societal acceptance will become hurdles.
Model and AI-powered product technologies are here, implementation of the technologies will take longer, and the process will be complex.
If you require data model development, deployment, verification, or validation, do not hesitate and contact us. We will also be glad to help you with your machine learning or artificial intelligence challenges when applied to asset management, trading, or risk evaluations.

Comments